Blog
Are psychedelics next to treat depression and PTSD?
Classic Psychedelics for the Treatment of Depressive Disorders: An Update for Psychiatrists in Training.
Abstract
In recent years, media and medical professionals have paid close attention to psychedelics as therapeutic agents. The evidence supporting the use of psychedelics in the treatment of major depressive disorder and treatment-resistant depression is updated for psychiatric trainees by the authors. Psilocybin, ayahuasca, lysergic acid diethylamide, and N,N-dimethyltryptamine are among the traditional, serotonergic psychedelics that have shown promise in numerous contemporary clinical trials for the treatment of depressive disorders. Larger, double-blinded trials should be used in future clinical trials to investigate the effectiveness of psychedelics and clarify severe adverse effects, psychedelics for depression online.
Recent years have seen a rise in interest in psychedelics among academics and the general public. Much of this attention has been drawn by reports of their numerous advantages for mood and overall health; recent research published in highly regarded journals, shop here.
psychedelics for depression Science Primer
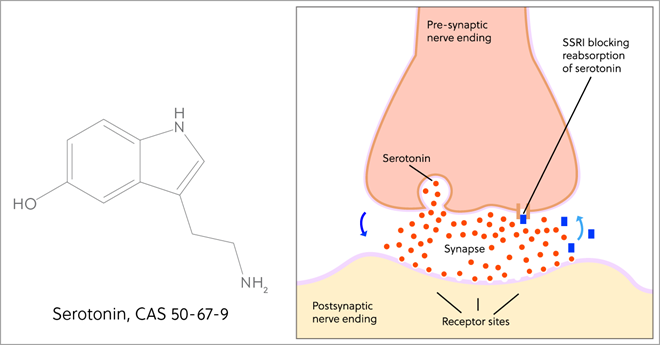
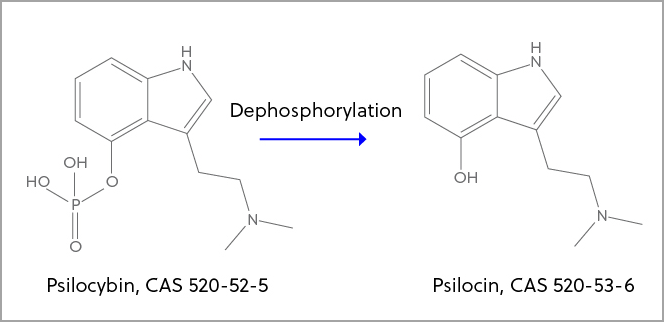
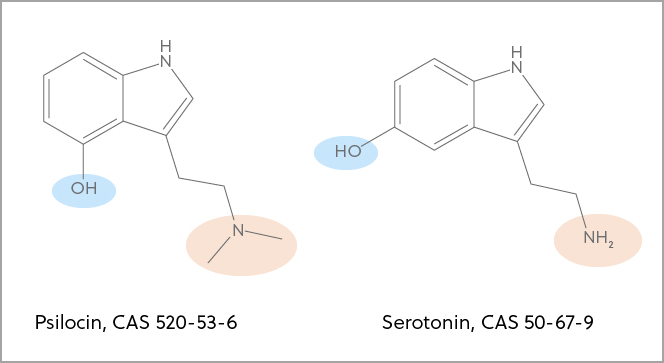
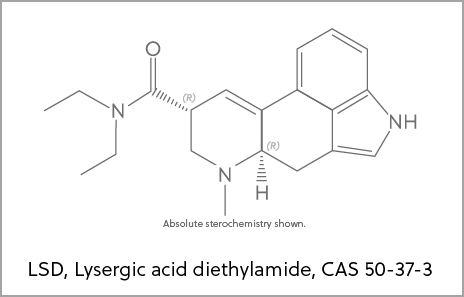
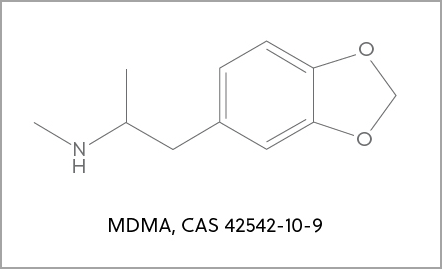
The serotonin 5-hydroxytryptamine 2A (also known as 5-HT2A) receptor is typically modulated by the serotonergic (“classic”) psychedelics (7). Psilocybin, lysergic acid diethylamide, ayahuasca, 5-methoxy-N,N-DMT, N,N-dimethyltryptamine (DMT), and mescaline are the most well-known substances in this class. There is continuous discussion about whether 5-HT2A receptor activity is necessary for a therapeutic effect, despite the fact that this receptor has been linked to the “mystical effects” of psychedelics (8). Nevertheless, some research indicates that alternative pharmacological pathways—such as altered default mode network function, heightened amygdala sensitivity, and reduced levels of inflammatory cytokines—might be accountable (9). On the other hand, because they do not function at the 5-HT2A receptor, “nonclassic” psychedelics like ketamine and 3,4-methylenedioxymethamphetamine are not covered in this article..
Psilocybin
Researchers saw immediate and long-lasting antidepressant effects in 24 patients with major depressive disorder in a 2021 randomized controlled trial when they administered moderate-dose (20 mg/70 kg) to high-dose (30 mg/70 kg) psilocybin (2). There was no statistically significant difference in the GRID-Hamilton Depression Rating Scale (GRID-HAM-D) scores of participants in the delayed treatment control group between the baseline and one and four weeks following the session. At weeks 1 and 4, over 70% of individuals in the psilocybin group experienced a clinically significant reduction (>50%) in their GRID-HAM-D scores (lower scores indicate less severe symptoms), with over 50% of them achieving remission. Comparable antidepressant effects were found in a reexamination conducted in 2022, which included a 12-month follow-up and had a sustained response rate of 75% and remission rate, click here for more on psychedelics for depression and other mental breakdowns.
Ayahuasca and N,N-DMT
Ayahuasca is a herbal beverage from South America that contains inhibitors of monoamine oxidase and DMT. The administration of ayahuasca to 17 participants with recurrent major depressive disorder and an average baseline mean HAM-D score of 19.24 was the subject of an uncontrolled open-label trial in 2016. The results showed that a single dose of ayahuasca produced a statistically significant decrease in the HAM-D score to 7.56 at day 21 (lower scores signal less severe symptoms) (15).
Researchers evaluated the effectiveness of single-dose ayahuasca versus placebo in a 2019 parallel-arm double-blind randomized controlled trial, which included 29 participants with TRD. Participants with psychotic disorders, bipolar disorders, or suicidal thoughts were not included. The ayahuasca group’s HAM-D scores changed seven days after treatment, reflecting significant effect sizes (16), get the best quality psychedelics for depression online.
Discussion of psychedelics for depression
Although these few preliminary studies are encouraging, they are still constrained by important design flaws such as expectancy bias, small sample sizes, and inadequate blinding. Larger sample sizes are required for better generalizability and the capacity to track side effects, even though the sample sizes were sufficient to detect statistical differences. Due to the strong subjective effects of psychedelics and expectancy bias from “trip-seeking” individuals, blinding has inherent challenges (11, 14, 18,). Whether blinding is a problem that can be solved is still up for debate. Concerns about blinding and bias may be lessened by the use of an active placebo, a reduction in the promotion of psychedelics in scientific circles and among the general public, and the employment of qualified raters (19). In psychedelic-assisted therapy, shop here.
Conclusion
Using psychedelics to treat depression has become a potentially effective treatment option. The research that are currently available, however, have important limitations. Larger double-blind clinical trials that investigate the effectiveness of psychedelics should uncover serious side effects..
Key Points/Clinical Pearls
-
Serotonergic psychedelics, primarily psilocybin, show promise in the treatment of major depressive disorder and treatment-resistant depression.
-
Despite promising results, modern clinical trials continue to be limited by relatively small samples and other design challenges.